
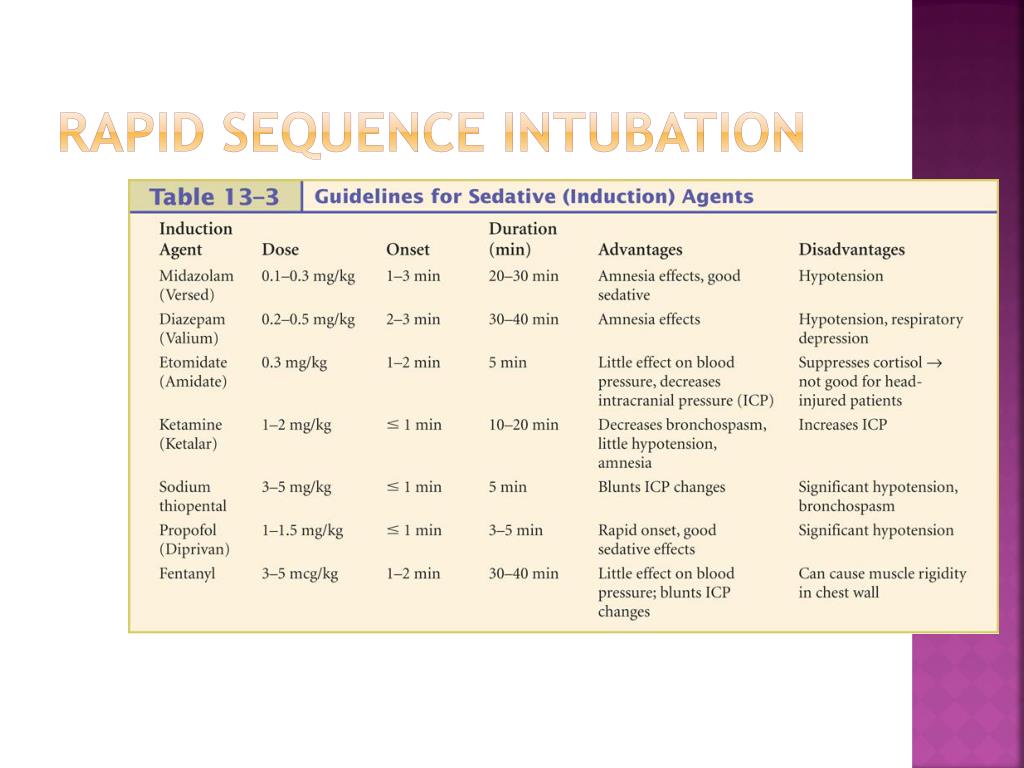
However, they state that some practioners use only rocuronium for all intubations. The authors recommend succylcholine unless there is a contraindication. It is immediately followed by IV push of a neuromuscular blocker, succinylcholine or rocuronium. The chapter is worth careful review.įirst an induction agent, often etomidate, is given by IV push. There are also times when the use of fentanyl may not be advisable (for example, in patients with sepsis or with compensated or decompensated shock). There are many details to the use of pretreatment medications which are covered in chapter 20 and should be carefully reviewed. When premedication is indicated, the drug or drugs, should be given 3 minutes before the induction agent and neuromuscular blocking agent. The ABC pneumonic refers to Asthma (reactive airways disease), Brain (increased intracranial pressure) and Cardiovascular (ischemic heart disease, hypertension, aortic dissection). Lidocaine is used for increased intracranial pressure or reactive airways disease. When pretreatment is indicated (the ABC pneumonic) fentanyl and/or lidocaine is used.įentanyl is used to blunt sympathetic response in, for example, patients with increased intracranial pressure, intracranial bleed, aortic dissection, and ischemic heart disease. These include marked sympathetic discharge causing increased heart rate and blood pressure, increase in intracranial pressure in patients with increased intracranial pressure, and bronchospasm.
Intubation and airway manipulation can have adverse physiologic effects on patients. Preoxygenation will be discussed in greater detail in an upcoming blog. Nasal cannula of 5 L per minute of oxygen provided during the intubation helps to delay oxygen desaturation during the intubation. We preoxygenate for three minutes or we can more rapidly achieve preoxygenation by asking the patient take eight vital capacity breaths of as close to 100% oxygen as our equipment permits (the patient breathes each breath as deeply as he can).Īn obese patient should be preoxygenated sitting up 30%. It is important to realize that the “100% non-rebreathing mask” delivers an oxygen concentration of at most 65 to 75%. We will administer to the spontaneously breathing patient an inhaled oxygen content that is as close to 100% as we can get. This will, again hopefully, prevent hypoxia and gastric aspiration. The purpose of this step is to use the lungs as an oxygen reservoir so that we, hopefully, do not need to use bag mask ventilation during the RSI.
RAPID SEQUENCE INTUBATION PROCESS FULL
The patient needs full monitoring of his vital signs including cardiac monitor, respiratory rate monitor, blood pressure monitor, pulse oximeter, and continuous wave capnography.Īll the medications need to be drawn up in syringes which are accurately labeled. The patient needs at least one or two secure intravenous lines in place. We assemble and check all the equipment that we might require. We will also make our plan for what we will do for a failed airway if that occurs. If the evaluation indicates a difficult airway, we will call for help and will use the difficult airway plan (perhaps an awake intubation if time permits. The first thing we do is to assess the patient for difficulty of intubation and for difficulty of bag mask ventilation if intubation fails. These are the steps we follow once the decision that intubation, for ventilatory support or for airway protection, is needed. RSI is a procedure with seven steps: The Seven Ps of RSI (1) In rapid sequence intubation we administer an induction agent, often etomidate, and a neuromuscular blocking agent (NMBA), succinylcholine or rocuronium, to render the patient unconscious and paralyzed for an emergency intubation after a period of preoxygenation and sometimes pretreatment with other medicines.


 0 kommentar(er)
0 kommentar(er)
